By Elizabeth Land Quant
On a December morning in 2017, I woke up face down next to my treadmill. The week before, a rheumatologist at Cleveland Clinic had diagnosed me with fibromyalgia, which she described as an “exercise depravation syndrome,” and told me that aerobic exercise would help my symptoms. “As long as your heart races a little and you sweat,” the doctor’s handout advised.
Now, as I lay on the floor, my heart raced like a trapped bird banging against my chest. I couldn’t take a deep breath. My pants were wet, from urine and sweat, and the nerves in my hands and feet were burning. I needed to throw up. Between the gray-tinged double vision and shaking in my legs, I couldn’t stand up, so I crawled across the floor and slowly pulled myself up the stairs.
After cleaning up my vomit, I vowed to follow my doctor’s advice and try even harder. Her handout said: “First, it is very important to know that even if the pain is worse after exercise, no injury to the body occurs.” But the next day when I tried to exercise things got worse. As the days wore on, I was unable to chew food. My neck muscles would not support my head, and I had to drink my dinner though a straw with my husband’s help. My chest hurt with every breath. I was incontinent, and my intestines became immobile. The burning in my hands and feet got so severe I couldn’t wear socks or gloves. My anxiety and depression were no longer controlled by my meds. I developed double vision and my left eye sagged. I couldn’t take care of my family anymore, or myself.
My husband worked a fulltime job, and we had three teenagers with medical and school needs. With my mother’s and sister’s help, we cobbled together a way to keep everyone fed, up on schoolwork, and attending most doctor’s appointments. Our daughter ran errands for the family after she got off work. My father-in-law picked up our boys from school as much as he could, with Uber as our back up. Dinner was made by anyone who had time that night, or we ordered. I missed countless school events like my son’s football games and my daughter’s high school homecoming coronation, memories we should have made together. I was so thankful that we could get by, but I constantly felt like a burden and a failure.
To get help, I traveled from my home in Minnesota to the Cleveland Clinic with the hope of finding answers for these symptoms. I chose this clinic because its website advertised a clinic that works “collaboratively with multiple consultants and departments.” But instead of finding answers, after I told her that some of these symptoms had started in childhood, my rheumatologist focused her questions on whether I was traumatized as a child. I didn’t know it at the time, but the rheumatologist that I was seeing is a renowned expert in fibromyalgia, and was head of the Fibromyalgia Clinic at Cleveland Clinic.
“You’ve got severe fibromyalgia. I’m recommending intense psychiatric rehabilitation,” she said.
I found out years later that this rheumatologist conducted a study on how past abuse can indicate the severity of fibromyalgia. Her conclusion was to “recommend that abuse should be inquired about in all patients evaluated for FMS as this may give more clarity to the nature and severity of the FMS presentation and prompt the need for psychological interventions.” This doctor also recommended that severe fibromyalgia patients should not be evaluated for other diseases.
Soon after, back in Minnesota, I was erroneously diagnosed with somatic symptom and related disorders (SSRD), a psychiatric condition that is “characterized by an intense focus on physical (somatic) symptoms that causes significant distress and/or interferes with daily functioning.” They claimed my symptoms were caused by a mental illness and not a physical disease.
For decades, my anxiety, depression and physical symptoms had been attributed by doctors to my own actions. For instance, I was told by a gastroenterologist that my inability to swallow food and my intestinal motility issues were most likely brought on by limiting certain foods from my diet, like gluten and dairy (but if I ate those foods, I got hives and threw up). Other doctors said that my symptoms were present because I “worked and exercised too much and didn’t rest,” or that I was “resting too much” and became deconditioned. I was scolded for being underweight. I was scolded for being overweight. I focused too much attention on my kids and not enough on myself, causing unneeded anxiety. Another doctor said that I focused too much on myself by meditating and googling which vitamins to take, causing an unhealthy obsession with my health. I was told that I just “didn’t like getting older” and was depressed about it. So, all my physical problems – double vision, throwing up, falling down, urinating all over myself – were my fault, and all my therapy sessions, meditation, medicine, exercise, and healthy diet weren’t helping nearly enough, and somehow were making me worse. I had wondered if my kids and husband would be better off without me.
***
I started researching my new diagnoses, and found out that the diagnostic criteria for fibromyalgia and SSRD placed a red flag on patients, primarily women, who have multiple symptoms. Because I fit the criteria for these two diagnoses, I was no longer a candidate for further testing or referral to other specialists. An article in the American Academy of Family Physicians’ magazine states that SSRD “should be considered early in the evaluation of patients with unexplained symptoms to prevent unnecessary interventions and testing.” With approximately 12 million US adults misdiagnosed every year, and women and minorities 20 to 30 percent more likely to be misdiagnosed, how many women are having their “unexplained symptoms” dismissed as part of a somatic illness?
How did we get to this point in the twenty-first century where women are still repeatedly dismissed and misdiagnosed? Women are less likely to be administered pain medicine than men in emergency room settings. Women have a 50% higher chance than men of getting an incorrect diagnosis after a heart attack, and they are 30 % more likely to have a stroke misdiagnosed. Black women and other women of color face even larger disparities in the health care system compared to white women because of racial bias and discrimination. Stigma and discrimination against Transgender people limit their access to healthcare, negatively affecting their mental and physical health. A study “Women With Pain” found that “women with chronic pain conditions are more likely to be wrongly diagnosed with mental health conditions than men and prescribed psychotropic drugs, as doctors dismissed their symptoms as hysterics.”
This brought me right back to college, where a professor asked the question “what is the Greek word for uterus?” When no one answered, he paused for a dramatic beat, and then said, “Hystera. Where we get the word hysteria.” As the women in the class shifted lower into their seats, the men laughed, loudly. There even was a celebratory high five. I will never forget the absolute mortification I felt, and how instinctively I hurried to cover my scars under my shirt from multiple endometriosis and ovarian cyst surgeries. I felt betrayed by my own body.
***
In ancient Egypt, Greece, and Rome, hysteria was considered a women’s condition whose physical symptoms were thought to be attributed to a wandering uterus. Over time, the blame of these various hysteria symptoms shifted from a physical cause to a mental one. In the late 1800’s, the psychoanalyst Sigmund Freud posited that a woman’s psychological stress “converted” into physical symptoms that caused a hysterical state. Also during the Victorian Era, new diagnostic terms like “Briquet’s Syndrome,” named after French physician Paul Briquet, were given to women experiencing hysteria symptoms such as nausea, dizziness, fast heartbeat, pain all over, blurry vision, and weakness. Briquet’s Syndrome was renamed somatization disorder, which eventually became somatic symptom and related disorders. Hysteria was officially removed from the Diagnostic and Statistical Manual of Mental Disorders in 1980, but the stigma of a woman’s illness with a name meaning “melodramatic or attention seeking behavior” still remains.
***
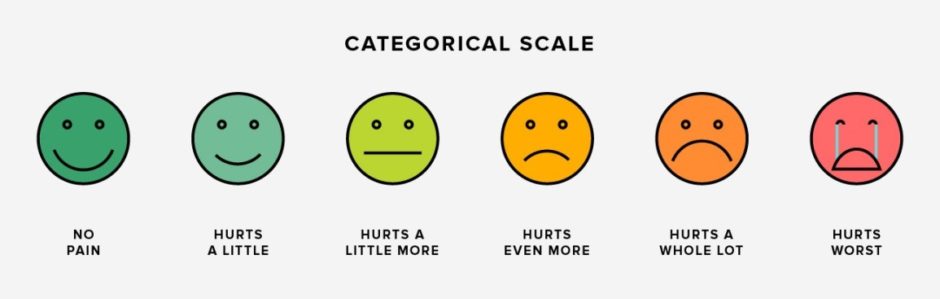
At numerous doctor’s appointments, I was given the Patient Health Questionnaire – 15 (PHQ-15), a tool frequently used to diagnose fibromyalgia, SSRD and multiple mental illnesses, which has symptoms that are also associated with diseases that primarily affect women. The tool listed 15 symptoms and a rating scale of how severely these symptoms affected your life. Each time I checked off most if not all of the symptoms listed, including chest pain, fatigue, heart pounding, nausea, pain, shortness of breath, and stomach pain (refer to chart for complete list). In filling out the PHQ-15, I thought I was helping the doctor get closer to a diagnosis and treatment. Instead, I was checking off a list of “somatic symptoms” that pointed them away from a physical illness and toward a psychiatric disorder like SSRD. Small fiber neuropathy, autoimmune disease, ovarian cancer, autonomic dysfunction, heart disease, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, Ehlers-Danlos syndromes, and now long-term Covid 19, conditions that affect millions of women, all have symptoms listed on the PHQ-15, and on screening questions for fibromyalgia. Another devastating problem with this set up is that more and more women are afraid of speaking up about their mental health symptoms, like I was, for fear of their physical symptoms being overlooked, or labelled as psychosomatic.
Women with mental illness, and I include myself in this group, are at risk of their mental health diagnoses being used as a red flag, halting the diagnostic process of their physical symptoms being looked into as part of a physical disease. More than 1 in 5 women in the US have experienced a mental health condition in the past year. In our modern understanding of mental health, we believe that physical symptoms often manifest as a result of a mental health disorder. The problem is not that doctors identify mental health disorders as one potential cause of physical symptoms. The problem is that those same physical symptoms could also be caused by a number of physical diseases. This is the point where the effective process of a proper diagnosis breaks down. Instead of testing and ruling out physical disease, many doctors jump to the assumption of the absence of physical disease. Having a mental illness does not make us immune to having a physical disease.
Seventy-five percent of Americans with autoimmune disease are women, according to the American Autoimmune Related Disease Association and it takes on average three years and four doctors to get a diagnosis of an autoimmune disease. The study “Frequency of Symptoms of Ovarian Cancer in Women Presenting to Primary Care Clinics” shows that even though 89% of women with early stages of ovarian cancer have a distinct set of symptoms (bloating, abdominal pain, urinary symptoms, fatigue, back pain, constipation) that they report to a doctor, “only 20% percent of cases are caught in an early stage.” How many of these women were dismissed by their doctors because their symptoms fit a somatic illness or were written off as general reproductive issues that halted further testing?
***
About a month after the Cleveland Clinic appointment, my family and I went on vacation in Florida. I almost didn’t go, but this was the only time we could coordinate a trip with all five of us. I spent most of my time in the bathroom, throwing up sips of water I kept trying to swallow. I took anti-nausea meds, Tylenol, Ativan and Imodium to sit with my family by the pool, until I would have to lie down on the bathroom tiles again.
By the time we flew home, I was severely dehydrated and doubled over in pain, but refused to go to the ER for fear I would be accused of faking my symptoms for attention or told that this was my fault and I needed to exercise more. My husband begged me to go in, and it was there that a doctor first mentioned “autonomic disorders,” and autoimmune nerve diseases that could be causing my various symptoms. When I got home from the hospital after getting IV fluids, I looked up my medical records from Cleveland Clinic. The doctor who diagnosed me with fibromyalgia wrote in my appointment notes, “has not been diagnosed with small fiber neuropathy,” a disease that could explain most of my symptoms. It would have been so easy for this rheumatologist to refer me to one of the few nerve labs in the country for a biopsy, right in her same clinic.
***
The diagnosis of fibromyalgia has helped many women get symptom relief and disability services, but has also prevented countless women from receiving a correct diagnosis. Studies show that half of fibromyalgia patients are thought to have small fiber neuropathy, a disease that Johns Hopkins describes as damage to the peripheral nervous system, the nerves that send information from the brain and spinal cord to the rest of the body. This damage can cause symptoms ranging from pain, to gastrointestinal issues, to difficulty breathing and an irregular heartbeat.
Fibromyalgia shares many of the same symptoms of small fiber neuropathy (SFN), but the main difference is that SFN can be definitively tested for and treated, whereas the underlying causes of fibromyalgia are unknown and treatments only address symptoms. A quick and painless skin biopsy can confirm the SFN diagnosis, and if positive, further diagnostics can find a medical cause of the neuropathy in the majority of patients. Prompt treatment can prevent further damage to the nerves, and in some cases, the medical cause of small fiber neuropathy can even be cured.
After researching my symptoms, I convinced an open-minded neurologist in Minneapolis to conduct testing including a skin biopsy and a tilt table test. The biopsy revealed severe small fiber neuropathy, and further testing found Post Orthostatic Tachycardia Syndrome (an autonomic disorder that affects heart rate, blood pressure, and causes many other symptoms). I was also diagnosed with Myasthenia Gravis, a progressive, potentially life-threatening neuromuscular disease which can be fatal with too much exertion (so much for “even if the pain is worse after exercise, no injury to the body occurs”). A year later I was diagnosed with a hypothyroid disorder and asthma, both of which I was told I have had for years. I could not have fought for and received the right tests if I didn’t have a good health care plan, time to research, and money to pay for thousands of dollars of out of pocket costs.
I had missed out on so many of my kids’ events, as well as countless birthdays, anniversaries and holidays. If I had been given a tilt table test or a nerve biopsy instead of being continually misdiagnosed, maybe I could have started the right medications and been more present in my children’s lives while they were still growing up.
***
Being disabled itself doesn’t upset or scare me. I learned that I can live a full and happy disabled life by watching my father work and travel the world with his portable oxygen tank in his backpack. I’m angry about all the time I wasted blaming myself for a disease that was not my fault and all the years fighting for tests and medicine that could have slowed down or stopped the progression of these diseases. However, I am privileged to have the resources I need to live a comfortable life that allows me time to take care of myself. It is unacceptable that in this country only well-to-do people with disabilities are able to live comfortably, while so many people are forced to fight to obtain correct diagnoses, assistance, adequate health care and safe housing.
When doctors are taught to hold back diagnostic testing based on the number of symptoms a patient has, and considering that so many illnesses that affect women have multiple symptoms, including potentially deadly ones like ovarian cancer, it’s not hard to understand why so many women have been misdiagnosed.
Elizabeth Land Quant is an autistic, queer, disabled writer, wife, and mom to three grown kids, two cats and a very spoiled dog. She studied Latin, Greek and political science at St. Olaf College, and splits her time between Minneapolis and Hot Springs, Arkansas. She researches and writes about her experiences with disability, autism, family, and her undying love for TV. Elizabeth writes poetry, fiction and nonfiction and is currently writing her first novel. She has been published in Disability Acts.
Anti-racist resources, because silence is not an option.
~~~~~~~~~~~~~~~~~~~~
Upcoming events with Jen
~~~~~~~~~~~~~~~~~~~~
THE ALEKSANDER SCHOLARSHIP FUND