“You have Fibro,” my doctor said three years ago. I wasn’t surprised. He suggested Gabapentin, Cymbalta, and a prescription NSAID and referred me to a rheumatologist. After years of unexplainable muscle pain, brain fog, and exhaustion, I finally had a diagnosis, like other conditions I’d accumulated since my twenties, some of which are Fibromyalgia-adjacent: namely IBS and Interstitial Cystitis—plus the umbrella culprit of lifelong anxiety.
For the next year and a half, my rheumatologist and I tried everything to ease my neurological suffering. All relevant medications and supplements for mental and physical health resulted in unmanageable side effects: shakiness, stomach pain, nausea, headaches, insomnia, worse anxiety, and depression. In the meantime, she sent me for nerve conduction testing and extensive blood tests to rule out autoimmune diseases. Everything checked out “normal.”
On my fifth visit to her office, I burst into tears. “I’m melting down!” I cried. She advised temporary disability, which my psychiatrist immediately obliged. I suddenly had time for an online meditation class and YouTube yoga. I embraced aquatic physical therapy, mental health therapy, and was relieved I was no longer required to check a sixteen-year-old work-related email inbox. I experienced stress relief, but the pain persisted.
While researching Ketamine, I read buzz-worthy articles about its advantages for depression, but I also learned it could work for chronic neuroplastic pain and anxiety disorders too. It felt like my final frontier. I scheduled six $750 treatments over a two-week period with a reputable clinic—the “magic number,” the doctor said—plus possible “boosters” later, all of which I couldn’t afford.
On treatment day one, the nurse called me “kiddo” as she apologized for slapping my wrist in search of a vein. My heart pounded, and my feet sweated inside my shoes.
“It’s like taking a nice long nap,” the nurse’s assistant said as she stuck sensors to my chest. I was skeptical.
“For the first treatment, we give you half the dose,” the nurse instructed. I wasn’t sure what that dose was. “You’re about to go on a beautiful journey” and be “one with the universe!”
She left me alone with my panic attack to watch my first hallucinogenic drug trip from the front desk via a small surveillance camera mounted to the ceiling.
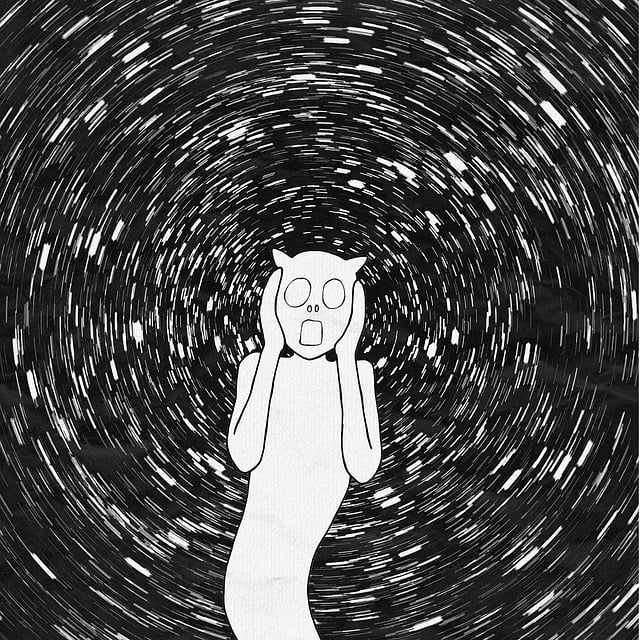
The tranquil spa music playing through giant headphones didn’t match my dread. I breathed deeply as a blood pressure cuff tightened around my bicep. I felt trapped. Within ten minutes, my body detached from my mind. A wave of nausea flowed through me, despite the antinausea medication mixed into the IV bag. I lifted my index finger to ascertain if I still had a body. For an instant, I was aware of it. Then it was gone again. Everything went black. The sleep mask over my eyes turned into a screen, my body no longer in the doctor’s office. I was in a blackout, aware of the blackout. The projector behind my eyes played a scene like lava flow. The molten charcoal and red magma rolled back and forth inside the mask. Conscious thoughts were fleeting.
When the Ketamine wore off an hour later, my head was bowling-ball heavy. Slowly my mind and body reconnected. My extremities buzzed with electricity, and I was still in pain.
The next afternoon, I returned thirsty, petrified, and still nauseous. I asked the doctor to increase the antinausea meds in the IV. The nurse once more struggled to find a vein and called me “kiddo.”
She realizes she’s several years younger than me, right? I thought.
At double the dose, grasping a conscious thought was an exercise in catching mist. This time the movie screen projecting from my eyes inside my mask consisted of a colorful video game of transmuting blocks. I awakened with the room spinning and an expanding purple bruise on my wrist.
Late that night, despite feeling like I had the flu, I noticed something astonishing: The pain I’d experienced every day for years was gone. I shook my shoulders and swiveled my neck. Nothing. It was a miracle. The powerful hallucinogen was supposedly lighting up long dormant neural pathways and forming new ones. Previously, I’d lie awake at night, marveling at the surging electricity in my limbs, pins and needles in my hands and feet. I’d awaken in the morning with stabbing lower back spasms and invisible knives embedded in the creases between my shoulders and neck. I woke up one morning with my bedroom floor a bed of nails against the soles of my feet. Ketamine turned my floor back into carpet.
But on treatment day three, my trepidation was all-consuming. When the nurse came into the room, I began to sob. “I’m scared,” I said. “I don’t want to do this again.”
“I’m sorry,” she said as she tried to find another vein. “Did you drink water?”
“Yes, up until two hours before, like you told me to,” I said.
“Why don’t I believe you?”
The blackout returned, but the colorful shapes didn’t. I was immersed in an obsidian void with a subconscious awareness the anguish would never end. I sensed my full bladder and suddenly felt as if I would pee in the chair before I regained my faculties. My lower half began to burn. At the end of the hour, the burning worsened. The nurse and her assistant returned.
“I have to pee so bad!” I screamed. “It burns!” I waved my arms above my lap.
They tried to lift me to a standing position, but I couldn’t walk. “My feet!”
“What about your feet?” the assistant asked.
“They’re . . . heavy!” I screamed.
“Moon boots. I know,” she said.
In the bathroom, as soon as I peed, the burning vanished. I’d hallucinated a UTI.
That night, unable to sleep because Ketamine is a mild stimulant, I Googled how long I would be pain-free after six treatments. Several clinics mentioned patients returning for another dose within weeks. I can’t go back, I thought.
I would only be pain-free for two weeks.
I longed to subdue my imbalanced brain. I yearned to extract the negative, repetitive thoughts and eradicate the real bodily pain that’s “all in my head.” Despite six months of guided meditation every day and four years of quality therapy, I essentially felt the same.
But a year and a half post-Ketamine, my hope was renewed when I discovered pain reprocessing therapy, which combines self-regulation exercises to retrain the brain and create new neural pathways without drugs. I downloaded the Curable app for an annual fee of $71.88. The introductory voice said, “Pain is an opinion.” I cried. With specific meditation, brain training, “somatic tracking,” writing exercises, and education about non-structural pain, I am experiencing glimmers of bodily progress reinforced by more than 24,000 people in the Curable Facebook community who attest to the benefits of long-term commitment. I woke up one morning with no lower back pain after a guide in the app told me, “Your pain is safe,” and asked me to reflect on it without fear.
Tamping down fear has always been the answer. There’s a strong link between perfectionism, people-pleasing, and physical pain, I’ve learned. The goal is to acknowledge the pain without sadness, anger, and more fear and conquer it with meaningful, mindful persistence. It will take longer than Ketamine, but it will be healthier and more permanent. A diagnosis wasn’t meaningful until I knew what to do with it. Now I do, and I’m finally ready for the self-directed process toward neurological well-being.
***
The ManifestStation publishes content on various social media platforms many have sworn off. We do so for one reason: our understanding of the power of words. Our content is about what it means to be human, to be flawed, to be empathetic. In refusing to silence our writers on any platform, we also refuse to give in to those who would create an echo chamber of division, derision, and hate. Continue to follow us where you feel most comfortable, and we will continue to put the writing we believe in into the world.
***
Our friends at Corporeal Writing are reinventing the writing workshop one body at a time.
Check out their current online labs, and tell them we sent you!
***
Silence is not an option, and inaction is collusion collusion